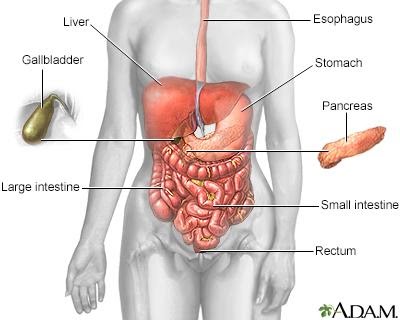
Hepatology is a branch of medicine concerned with the study, prevention, diagnosis and management of diseases that affect the liver, gallbladder, biliary tree and pancreas. The term hepatology is derived from the Greek words “hepatikos” and “logia,” which mean liver and study, respectively.
Hepatitis affects millions of individuals globally and is associated with several poor outcomes including liver transplant and liver cancer. In particular, hepatitis B and hepatitis C are major causes of liver cancer, while alcohol abuse has been linked to conditions such as cirrhosis and other serious complications. The conditions hepatologists deal with most frequently are viral hepatitis and alcohol-related liver disease.
Some of the most common ailments that are assessed, diagnosed and managed by a hepatologist include:
- Diseases of the liver related to excess alcohol consumption, including fatty liver disease, liver cirrhosis and liver cancer.
- Viral hepatitis infections (hepatitis A, B, C and E). Over two billion individuals have been infected with hepatitis B at some point and around 350 million people are persistent carriers. With widespread vaccination and blood screening, the incidence of hepatitis B has significantly decreased. However, hepatitis B and hepatitis C are accountable for up to 80% of liver cancer cases.
- Drug overdose, particularly paracetamol overdose
- Jaundice
- Gastrointestinal bleeding caused by portal hypertension linked to liver injury
- Enzyme defects causing liver enlargement in children, also known of as liver storage diseases
- Some tropical infections such as hydatid cyst, kala-azar or schistosomiasis
- Liver transplantation
- Liver cancer
- Genetic and metabolic liver disease
- Pancreatitis, usually when caused by alcohol consumption or gallstones
- Drug metabolism
- Damage to the pancreas or biliary tract caused by infection, cancer, alcohol, bleeding or obstruction.

Hepatology used to be considered a subspecialty of gastroenterology, but nowadays doctors can specialize in hepatology, which is quickly emerging as a freestanding speciality. As a critical organ that can be affected by a large number of factors, the liver is usually the focal point in hepatology.
A hepatologist generally only assesses patients after they are referred by their doctor. A hepatologist may also be involved in the follow-up of patients who have received a liver transplant.
Some of the procedures hepatologists are required to perform include the following:
- Endoscopic retrograde cholangiopancreatography, which is used to diagnose and treat many biliary and pancreatic diseases.
- Transhepatic pancreato-cholangiography, whichis an X-ray used to detect obstruction in the bile ducts or liver.
- Transjugular intrahepatic portosystemic shunt, an artificial channel made to create a connection between the portal and hepatic veins.
In addition to caring for patients, a hepatologist may be involved in research looking at novel therapeutic approaches to disease or prevention methods such as screening, for example.
Hepatology is the branch of medicine that incorporates the study of liver, gallbladder, biliary tree, and pancreas as well as management of their disorders. Details are as follows.
The human liver is an organ that has many functions and jobs within the body. It is a part of the digestive system, and it is responsible for everything from cholesterol production to waste filtering. It is vitally important to overall health and should be taken care of to avoid life-threatening diseases that can develop if a liver becomes overworked or unhealthy.
FUNCTION
The liver is a part of the digestive system, but it does much more than simply process food intake. It is responsible for producing substances that will break down fats and lipids, making foods more digestible. It also produces several amino acids, which are essential to protein production, without which a body could not function. The liver produces much of the cholesterol in a body, whether healthy or unhealthy. Aside from the liver’s production abilities, it also acts as a filter. When a harmful substance is taken into the body, the liver is the organ responsible for filtration. For example, the liver filters alcohol out of the blood. Simply stated, the main function of the liver is to keep an equilibrium in the body. It neutralizes toxins that are harmful, it creates substances that are necessary and it disposes of waste products.
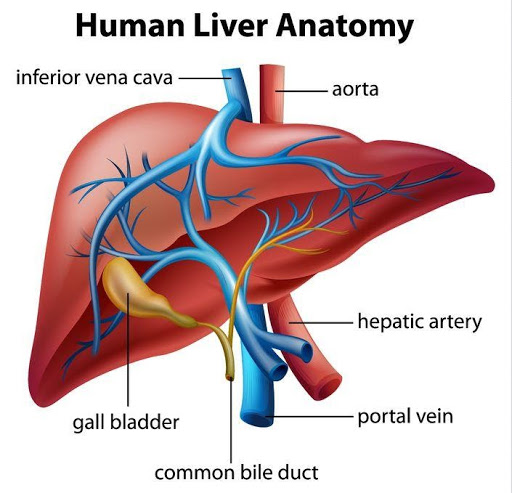
FEATURES
The liver is composed of an intricate network of blood vessels, capillaries and metabolic cells. The two major blood vessels connected to the liver, the hepatic artery and the portal vein, are responsible for carrying blood to the liver. The hepatic artery brings oxygenated blood from the heart so that the liver stays healthy and functioning. The portal vein brings blood with digested food particles in it from the small intestines, which the liver then filters and turns into carbohydrates, amino acids or waste products. The actual production of essential chemicals happens in the metabolic cells, which are grouped together in structures called lobules. There are thousands of these lobules in the liver, all of which work to produce and filter different substances.
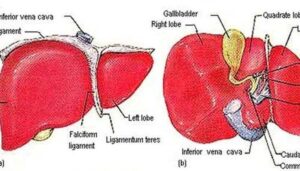
IDENTIFICATION
The liver is a reddish-brown organ that is found on the right side of the abdominal cavity, just underneath the diaphragm. The coloring of the liver can be explained because of the great amount of blood being transported through it continuously. It is wedge-shaped, it usually weighs about 3 lbs. and it is divided into four lobes. These lobes are different shapes and sizes, and they are responsible for different functions within the liver. These lobes are called the right lobe, the left lobe, the quadrate lobe and the caudate lobe. They are separated and held together by ligaments and connective tissue.
DISEASES
Since the liver is an organ that has potentially hundreds of tasks to complete, and since it deals with complex and sometimes dangerous chemicals, diseases of the liver can be common. The most common of these diseases is cirrhosis, which is a scarring and hardening of liver tissue. Cirrhosis is caused by bacterial or viral infections, but also by alcohol abuse. Cirrhosis leads to an inability of the liver to function properly. In these cases, the liver will eventually become unable to produce the proteins that the body needs, and it will be unable to filter out toxins. Hepatitis, another common liver disease, is an inflammation of the liver that is caused by either a viral infection or alcohol abuse. Drugs can also cause major liver problems, since an overdose of drugs will overwhelm the liver and it will not be able to fully filter out toxins. Many of these diseases and conditions will eventually lead to liver failure, the only known cure for which is a liver transplant.
POTENTIAL
In recent years, there has been an emphasis in the medical community on finding more effective forms of liver transplants for patients with liver failure. Aside from traditional liver transplants, which can sometimes be rejected by the bodies of patients, other alternatives have been developed which incorporate both biological and non-biological elements. For example, along with a standard liver transplant, a non-biological system can be used to help in the filtration duties of a new or damaged liver. Biological approaches are also being developed. These include partial transplants, which would mean that a living donor could give a portion of their healthy liver to a patient with liver failure. It has also been suggested that the livers of pigs, which have similar organ structures to those of humans, could be used in situations where a human liver donation cannot be acquired in time. These techniques, and many others, are being researched and perfected.
GALLBLADDER :
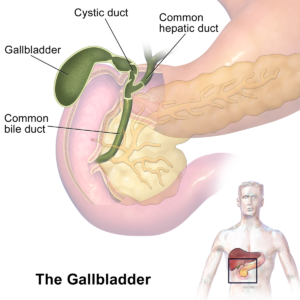
In vertebrates the gallbladder (also gall bladder, biliary vesicle or cholecyst) is a small organ where bile (a fluid produced by the liver) is stored and concentrated before it is released into the small intestine. Humans can live without a gallbladder. The surgical removal of the gallbladder is called a cholecystectomy.
Structure :
The gallbladder is a hollow organ that sits just beneath the right lobe of the liver. In adults, the gallbladder measures approximately 8 centimetres (3.1 inches) in length and 4 centimetres (1.6 in) in diameter when fully distended. The gallbladder has a capacity of about 100 millilitres (3.5 imperial fluid ounces).
The gallbladder is shaped like a tapered sac, with the open end opening into the biliary tree and the cystic duct. Anatomically, the gallbladder is divided into three sections: the fundus, body, and neck: The fundus is a rounded end that faces the front of the body. The body is in contact with the liver, lying in the gallbladder fossa, a depression at the bottom of the liver. The neck tapers and is continuous with the cystic duct, part of the biliary tree. The gallbladder fossa, against which the fundus and body of the gallbladder lie, is found beneath the junction of hepatic segments IVB and V. The cystic duct unites with the common hepatic duct to become the common bile duct. At the junction of the neck of the gallbladder and the cystic duct, there is an out-pouching of the gallbladder wall forming a mucosal fold known as Hartmann’s pouch, where gallstones commonly get stuck.
The angle of the gallbladder is located between the costal margin and the lateral margin of the rectus abdominis muscle. The fundus is at the same level as the transpyloric plane.
DEVELOPMENT
The gallbladder develops from an endodermal outpouching of the embryonic gut tube. Early in development, the human embryo has three germ layers and abuts an embryonic yolk sac. During the second week of embryogenesis, as the embryo grows, it begins to surround and envelop portions of this sac. The enveloped portions form the basis for the adult gastrointestinal tract. Sections of this foregut begin to differentiate into the organs of the gastrointestinal tract, such as the oesophagus, stomach, and intestines.
During the fourth week of embryological development, the stomach rotates. The stomach, originally lying in the midline of the embryo, rotates so that its body is on the left. This rotation also affects the part of the gastrointestinal tube immediately below the stomach, which will go on to become the duodenum. By the end of the fourth week, the developing duodenum begins to spout a small outpouching on its right side, the hepatic diverticulum, which will go on to become the biliary tree. Just below this is a second outpouching, known as the cystic diverticulum, that will eventually develop into the gallbladder.
VARIATION
Anatomical variants of the gallbladder occur very rarely, although a range of abnormalities have been documented.
The number and structure of the gallbladder may vary. Occasionally two or even three gallbladders may coexist, either as separate bladders draining into the cystic duct, or sharing a common branch that drains into the cystic duct. Additionally, the gallbladder may fail to form at all. Gallbladders with two lobes separated by a septum may also exist. These abnormalities are not likely to affect function and are generally asymptomatic.
The location of the gallbladder in relation to the liver may also vary, with documented variants including gallbladders found within, above, on the left side of, behind, and detached from the liver. Such variants are very rare: from 1886 to 1998, only 110 cases of left-lying liver, or less than one per year, were reported in scientific literature.
An anatomical variation can occur, known as a Phrygian cap, which is an innocuous fold in the fundus, named after its resemblance to the Phrygian cap.[16]
FUNCTION :
The main purpose of the gallbladder is to store bile, also called gall, needed for the digestion of food. The gallbladder is part of the biliary system and serves as a reservoir for bile, which is produced by the liver. The liver produces the bile, which then flows through the hepatic ducts into the gallbladder. At any one time, 30 to 60 millilitres (1.0 to 2.0 US fl oz) of bile is stored within the gallbladder.[17]
When food containing fat enters the digestive tract, it stimulates the secretion of cholecystokinin (CCK) from I cells of the duodenum and jejunum. In response to cholecystokinin, the gallbladder rhythmically contracts and releases its contents into the common bile duct, eventually draining into the duodenum. The bile emulsifies fats in partly digested food, thereby assisting their absorption. Bile consists primarily of water and bile salts, and also acts as a means of eliminating bilirubin, a product of hemoglobin metabolism, from the body.[17]
The bile that is secreted by the liver and stored in the gallbladder is not the same as the bile that is secreted by the gallbladder. During gallbladder storage of bile, it is concentrated by removal of some water and electrolytes. This is through the active transport of sodium ions across the epithelia of the gallbladder, which creates an osmotic pressure that also causes water and other electrolytes such as chloride to be reabsorbed.
CLINICAL SIGNIFICANCE
GALLSTONES
Gallstones are the most common problem to affect the gallbladder. Gallstones generally form when the bile is saturated with either cholesterol or bilirubin. Only a minority of gallstones cause symptoms; most stones are passed along the biliary system. When symptoms occur, severe pain in the upper right part of the abdomen is felt. If the stone blocks the gallbladder, inflammation as cholecystitis may result. If the stone lodges in the biliary system, jaundice may occur; and if the stone blocks the pancreatic duct, then pancreatitis may occur. Gallstones are often managed by waiting for them to be naturally passed. In people with recurrent gallstones, surgery to remove the gallbladder may be considered. Some medication, such as ursodeoxycholic acid, may be used; and lithotripsy, a procedure used to break down the stones, may also be used.
INFLAMMATION
Inflammation of the gallbladder is known as cholecystitis. Inflammation is commonly caused by obstruction of the duct with gallstones, which is known as cholelithiasis. Blocked bile accumulates, and pressure on the gallbladder wall may lead to the release of substances that cause inflammation, such as phospholipase. There is also the risk of bacterial infection. An inflamed gallbladder is likely to cause pain and fever, and tenderness in the upper, right corner of the abdomen, and may have a positive Murphy’s sign. Cholecystitis is often managed with rest and antibiotics, particularly cephalosporins and, in severe cases, metronidazole.[19]
Cholecystitis may also occur chronically, particularly when a person is prone to getting gallstones.
CHOLESTEROLOSIS
Cholesterolosis of the gallbladder, also called strawberry gallbladder, is a change in the gallbladder wall due to excess cholesterol.[20] It is not linked to gallstones or inflammation.
Gallbladder polyps
Gallbladder polyps are mostly benign growths or lesions resembling growths that form in the gallbladder wall.[21]
Gallbladder removal
Main article: Cholecystectomy
A cholecystectomy is a procedure in which the gallbladder is removed. It may be removed because of recurrent gallstones, and is considered an elective procedure. A cholecystectomy may be an open procedure, or one conducted by laparoscopy. In the surgery, the gallbladder is removed from the neck to the fundus,[22] and so bile will drain directly from the liver into the biliary tree. About 30 percent of patients may experience some degree of indigestion following the procedure, although severe complications are much rarer.[19]
About 10 percent of surgeries lead to a chronic condition of postcholecystectomy syndrome.[23]
Imaging

Ultrasound of a gallbladder with a large gallstone
Ultrasound is often the first imaging examination performed when galbladder disease is suspected. Other imaging options include MRCP (magnetic resonance cholangiopancreatography), ERCP and percutaneous or intraoperative cholangiography. A cholescintigraphy scan is a nuclear imaging procedure used to assess the condition of the gallbladder.
Biliary tract
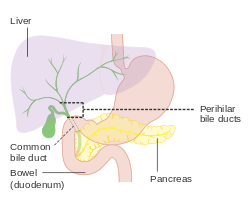
The biliary tract, (biliary tree or biliary system) refers to the liver, gall bladder and bile ducts, and how they work together to make, store and secrete bile. Bile consists of water, electrolytes, bile acids, cholesterol, phospholipids and conjugated bilirubin. Some components are synthesised by hepatocytes (liver cells), the rest are extracted from the blood by the liver.
Bile is secreted by the liver into small ducts that join to form the common hepatic duct. Between meals, secreted bile is stored in the gall bladder. During a meal, the bile is secreted into the duodenum to rid the body of waste stored in the bile as well as aid in the absorption of dietary fats and oils.
Structure
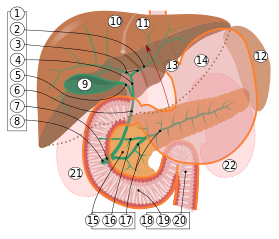
- Bile ducts: 2. Intrahepatic bile ducts, 3. Left and right hepatic ducts, 4. Common hepatic duct, 5. Cystic duct, 6. Common bile duct, 7. Ampulla of Vater, 8. Major duodenal papilla
9. Gallbladder, 10–11. Rightand left lobes of liver. 12. Spleen.
13. Esophagus. 14. Stomach. 15. Pancreas: 16: Accessory pancreatic duct, 17: Pancreatic duct.
18. Small intestine: 19. Duodenum, 20. Jejunum
21–22: Right and left kidneys (silhouette).
The anterior border of the liver is lifted upwards (brown arrow). Gallbladder with Longitudinal section, pancreas and duodenum with frontal one. Intrahepatic ducts and stomach in transparency.
The biliary tract is the common anatomical term for the path by which bile is secreted by the liver then transported to the first part of the small intestine, also known as the duodenum. A structure common to most members of the mammal family, it is often referred to as a tree because it begins with many small branches which end in the common bile duct, sometimes referred to as the trunk of the biliary tree. The duct, the branches of the hepatic artery, and the portal vein form the central axis of the portal triad. Bile flows in the direction opposite to that of the blood present in the other two channels.
The system is usually referred to as the biliary tract or system, and can include the use of the term hepatobiliary when used to refer just to the liver and bile ducts. The name biliary tract is used to refer to all of the ducts, structures and organs involved in the production, storage and secretion of bile.
The path is as follows:
Bile canaliculi >> Canals of Hering >> intrahepatic bile ductule (in portal tracts / triads) >> interlobular bile ducts >> left and right hepatic ducts >>
merge to form >> common hepatic duct >>
exits liver and joins >> cystic duct (from gall bladder) >>
forming >> common bile duct >> joins with >> pancreatic duct >>
forming >> ampulla of Vater >> enters duodenum
Function
Bile is secreted by the liver into small ducts that join to form the common hepatic duct. Between meals, secreted bile is stored in the gall bladder, where 80%-90% of the water and electrolytes can be absorbed, leaving the bile acids and cholesterol. During a meal, the smooth muscles in the gallbladder wall contract, leading to the bile being secreted into the duodenum to rid the body of waste stored in the bile as well as aid in the absorption of dietary fats and oils by solubilizing them using bile acids.
Clinical significance
Pressure inside in the biliary tree can give rise to gallstones and lead to cirrhosis of the liver.
The biliary tract can also serve as a reservoir for intestinal tract infections. Since the biliary tract is an internal organ, it has no somatic nerve supply, and biliary colic due to infection and inflammation of the biliary tract is not a somatic pain. Rather, pain may be caused by luminal distension, which causes stretching of the wall. This is the same mechanism that causes pain in bowel obstructions.
An obstruction of the biliary tract can result in jaundice, a yellowing of the skin and whites of the eyes
Pancreas :
The pancreas /ˈpæŋkriəs/ is a glandular organ in the digestive system and endocrine system of vertebrates. In humans, it is located in the abdominal cavity behind the stomach. It is an endocrine gland producing several important hormones, including insulin, glucagon, somatostatin, and pancreatic polypeptide which circulate in the blood. The pancreas is also a digestive organ, secreting pancreatic juicecontaining digestive enzymes that assist digestion and absorption of nutrients in the small intestine. These enzymes help to further break down the carbohydrates, proteins, and lipids in the chyme. The pancreas is also known as a mixed gland
Structure
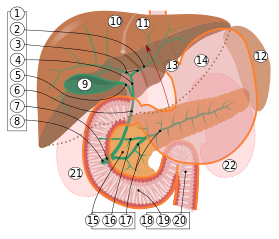
- Bile ducts: 2. Intrahepatic bile ducts, 3. Left and right hepatic ducts, 4. Common hepatic duct, 5. Cystic duct, 6. Common bile duct, 7. Ampulla of Vater, 8. Major duodenal papilla
9. Gallbladder, 10–11. Rightand left lobes of liver. 12. Spleen.
13. Esophagus. 14. Stomach. 15. Pancreas: 16: Accessory pancreatic duct, 17: Pancreatic duct.
18. Small intestine: 19. Duodenum, 20. Jejunum
21–22: Right and left kidneys (silhouette).
The anterior border of the liver is lifted upwards (brown arrow). Gallbladder with Longitudinal section, pancreas and duodenum with frontal one. Intrahepatic ducts and stomach in transparency.
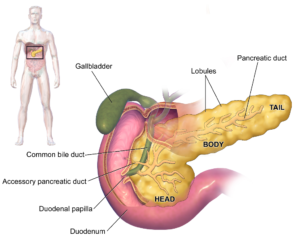
The pancreas is an endocrine and digestive organ that, in humans, lies in the upper left part of the abdomen. It is found behind the stomach.[2] The pancreas is about 15 cm (6 in) long.[3]
Anatomically, the pancreas is divided into the head of pancreas, the neck of pancreas, the body of pancreas, and the tail of pancreas. The head is surrounded by the duodenum in its concavity. The head surrounds two blood vessels, the superior mesenteric artery and vein. From the back of the head emerges a small uncinate process which extends to the back of the superior mesenteric vein and ends at the superior mesenteric artery.[4] The neck is about 2.5 cm long and lies between the head and the body, and in front of the superior mesenteric artery and vein. Its front upper surface supports the pylorus (the base) of the stomach. The neck arises from the left upper part of the front of the head. It is directed at first, upward and forward, and then upward and to the left to join the body; it is somewhat flattened from above downward and backward. On the right it is grooved by the gastroduodenal artery. The body is the largest part of the pancreas and lies behind the pylorus, at the same level as the transpyloric plane.[5] The tail ends by abutting the spleen.
The pancreas is a secretory structure with an internal hormonal role (endocrine) and an external digestive role (exocrine). It has two main ducts, the main pancreatic duct, and the accessory pancreatic duct. These drain enzymes through the ampulla of Vater into the duodenum.[6]
Margins
The upper margin of the pancreas is blunt and flat to the right; narrow and sharp to the left, near the tail.
It begins on the right in the omental tuber, and is in relation with the celiac artery, from which the hepatic artery courses to the right just above the gland, while the splenic artery runs toward the left in a groove along this border.
The lower margin of the pancreas separates the posterior from the inferior surface; the superior mesenteric vessels emerge under its right extremity.
The frontal margin of the pancreas separates the anterior from the inferior surface of the pancreas, and along this border the two layers of the transverse mesocolon diverge from one another; one passing upward over the frontal surface, the other backward over the inferior surface.
Surfaces
The inferior surface of the pancreas is narrow on the right but broader on the left, and is covered by peritoneum; it lies upon the duodenojejunal flexure and on some coils of the jejunum; its left extremity rests on the splenic flexure of the colon.
The anterior surface of the pancreas faces the front of the abdomen. Most of the right half of this surface is in contact with the transverse colon, with only areolar tissue intervening.
From its upper part it joins to the neck of the pancreas at a well-marked prominence, the omental tuber which abuts the lesser omentum. Its right edge is marked by a groove for the gastroduodenal artery.
The lower part of the right half, below the transverse colon, is covered by peritoneum continuous with the inferior layer of the transverse mesocolon, and is in contact with the coils of the small intestine.
The superior mesenteric artery passes down in front of the left half across the uncinate process; the superior mesenteric vein runs upward on the right side of the artery and, behind the neck, joins with the lienal vein to form the portal vein.
Blood supply
The pancreas receives blood from branches of both the coeliac artery and superior mesenteric artery. The splenic artery runs along the top margin of the pancreas, and supplies the neck, body and tail of the pancreas through its pancreatic branches, the largest of which is called the greater pancreatic artery. The superior and inferior pancreaticoduodenal arteries run along the anterior and posterior surfaces of the head of the pancreas at its border with the duodenum. These supply the head of the pancreas.
The body and neck of the pancreas drain into the splenic vein; the head drains into the superior mesenteric and portal veins.
Histology :
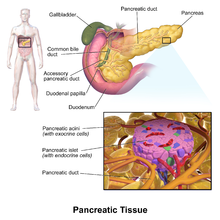
Pancreatic tissue, including a pancreatic islet
The pancreas contains tissue with an endocrine and exocrine role, and this division is also visible when the pancreas is viewed under a microscope.
The tissues with an endocrine role can be seen under staining as lightly-stained clusters of cells, called pancreatic islets (also called islets of Langerhans).
Darker-staining cells form clusters called acini, which are arranged in lobes separated by a thin fibrous barrier. The secretory cells of each acinus surround a small intercalated duct. Because of their secretory function, these cells have many small granules of zymogens that are visible. The intercalated ducts drain into larger ducts within the lobule, and finally interlobular ducts. The ducts are lined by a single layer of columnar epithelium. With increasing diameter, several layers of columnar cells may be seen.
Variation:
The size of the pancreas varies considerably. Several anatomical variations exist, relating to the embryological development of the two pancreatic buds. The pancreas develops from these buds on either side of the duodenum. The ventral bud eventually rotates to lie next to the dorsal bud, eventually fusing. If the two buds each having a duct, do not fuse, a pancreas may exist with two separate ducts, a condition known as a pancreas divisum. This condition has no physiologic consequence. If the ventral bud does not fully rotate, an annular pancreas may exist. This is where sections of the pancreas completely encircle the duodenum, and may even lead to duodenal atresia.
An accessory pancreatic duct may exist if the main duct of pancreas does not regress.
Development
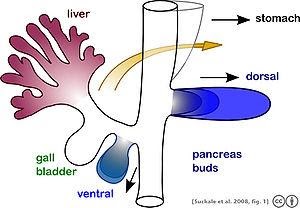
Schematic illustrating the development of the pancreas from a dorsal and a ventral bud. During maturation, the ventral bud flips to the other side of the gut tube (arrow) where it typically fuses with the dorsal lobe. An additional ventral lobe that usually regresses during development is omitted.
As part of embryonic development the pancreas forms from the embryonic foregut and is therefore of endodermal origin. Pancreatic development begins with the formation of a ventral and a dorsal pancreatic bud. Each structure communicates with the foregut through a duct. The dorsal pancreatic bud forms the head, neck, body, and tail, whereas the ventral pancreatic bud forms the uncinate process.[8]
Differential rotation and fusion of the ventral and dorsal pancreatic buds results in the formation of the definitive pancreas.[9] As the duodenum rotates to the right, it carries with it the ventral pancreatic bud and common bile duct. Upon reaching its final destination, the ventral pancreatic bud fuses with the much larger dorsal pancreatic bud. At this point of fusion, the main ducts of the ventral and dorsal pancreatic buds fuse, forming the main pancreatic duct. The duct of the dorsal bud regresses, leaving the main pancreatic duct.[8]
Differentiation of cells of the pancreas proceeds through two different pathways, corresponding to the dual endocrine and exocrine functions of the pancreas. In progenitor cells of the exocrine pancreas, important molecules that induce differentiation include follistatin, fibroblast growth factors, and activation of the Notch receptor system.[9] Development of the exocrine acini progresses through three successive stages. These are the predifferentiated, protodifferentiated, and differentiated stages, which correspond to undetectable, low, and high levels of digestive enzyme activity, respectively.
The multipotent pancreatic progenitor cells have the capacity to differentiate into any of the pancreatic cells: acinar cells, endocrine cells, and ductal cells. These progenitor cells are characterised by the co-expression of the transcription factors PDX1 and NKX6-1. Under the influence of neurogenin-3and ISL1, but in the absence of notch receptor signaling, these cells differentiate to form two lines of committed endocrine precursor cells. The first line, under the direction of a Pax gene, forms α- and γ- cells, which produce glucagon and pancreatic polypeptides, respectively. The second line, influenced by Pax-6, produces beta cells (β-) and delta cells (δ-), which secrete insulin and somatostatin, respectively.
Insulin and glucagon can be detected in the human fetal circulation by the fourth or fifth month of fetal development.
Function
The pancreas is involved in blood sugar control and metabolism within the body, and also in the secretion of substances (collectively pancreatic juice) which help digestion. Classically, these are divided into an “endocrine” role, relating to the secretion of [insulin] and other substances within pancreatic islets and helping control blood sugar levels and metabolism within the body, and an “exocrine” role, relating to the secretion of enzymes involved in digesting substances from outside of the body.
Sugar control and metabolism :

Blood glucose levels are maintained at a constant level in the body by a negative feedback mechanism. When the blood glucose level is too high, the pancreas secretes insulin and when the level is too low, the pancreas then secretes glucagon. The flat line shown represents the homeostatic set point. The sinusoidal line represents the blood glucose level.
Approximately 3 million cell clusters called pancreatic islets are present in the pancreas.[10] Within these islets are four types of cells which are involved in the regulation of blood glucose levels. Each type of cell secretes a different type of hormone: α alpha cells secrete glucagon(increase glucose in blood), β beta cells secrete insulin (decrease glucose in blood), δ delta cells secrete somatostatin (regulates/stops α and β cells) and PP cells, or γ (gamma) cells, secrete pancreatic polypeptide.[11] These act to control blood glucose through secreting glucagon to increase the levels of glucose, and insulin to decrease it.
The islets are crisscrossed by a dense network of capillaries. The capillaries of the islets are lined by layers of islet cells, and most endocrine cells are in direct contact with blood vessels, either by cytoplasmic processes or by direct apposition. The islets function independently from the digestive role played by the majority of pancreatic cells.[12]
Activity of the cells in the islets is affected by the autonomic nervous system:
Sympathetic (adrenergic)
α2: decreases secretion from beta cells, increases secretion from alpha cells, β2: increases secretion from beta cells
Parasympathetic (muscarinic)
M3: increases stimulation of alpha cells and beta cells[13]
Digestion
The pancreas plays a vital role in the digestive system. It secretes fluid that contains enzymes into the duodenum. These enzymes help to break down carbohydrates (usually starch), proteins and lipids (fats). This role is called the “exocrine” role of the pancreas. Cells are arranged clusters called acini. Secretions into the middle of the acinus accumulate in intralobular ducts that drain to the main pancreatic duct, which drains directly into the duodenum.
The cells are filled with granules containing the digestive enzymes. These are secreted in an inactive form called (termed zymogens or proenzymes). When released into the duodenum, they are activated by the enzyme enteropeptidase present in the lining of the duodenum. The proenzymes are cleaved, creating a cascade of activating enzymes: enteropeptidase activates the proenzyme trypsinogen by cleaving it to form trypsin. The free trypsin then cleaves the rest of the trypsinogen, as well as chymotrypsinogen to its active form chymotrypsin.
The pancreas secretes substances which help in the digestion of starch and other carbohydrates, proteins and fats.[14] Proteases, the enzymes involved in the digestion of proteins, include trypsinogen and chymotrypsinogen. The enzyme involved in the digestion of fats is lipase. Amylase, also secreted by the pancreas, breaks down starch (amylum) and other carbohydrates. The pancreas also secretes phospholipase A2, lysophospholipase, and cholesterol esterase.
Secretion of these proenzymes is via the hormones gastrin, cholecystokinin and secretin, which are secreted by cells in the stomach and duodenum in response to distension and/or food.
Clinical significance
Histology :

Pancreas parts
Pancreatic disease
A perforation of the pancreas, which may lead to the secretion of digestive enzymes such as lipase and amylase into the abdominal cavity as well as subsequent pancreatic self-digestion and digestion and damage to organs within the abdomen, generally requires prompt and experienced medical intervention.
It is possible for one to live without a pancreas, provided that the person takes insulin for proper regulation of blood glucose concentration and pancreatic enzyme supplements to aid digestion.[15]
Inflammation
Inflammation of the pancreas is known as pancreatitis. Pancreatitis is most often associated with recurrent gallstones or chronic alcohol use, although a variety of other causes, including measles, mumps, some medications, the congenital condition alpha-1 antitrypsin deficiency and even some scorpion stings, may cause pancreatitis. Pancreatitis is likely to cause intense pain in the central abdomen, that often radiates to the back, and may be associated with jaundice. In addition, due to causing problems with fat digestion and bilirubinexcretion, pancreatitis often presents with pale stools and dark urine.
In pancreatitis, enzymes of the exocrine pancreas damage the structure and tissue of the pancreas. Detection of some of these enzymes, such as amylase and lipase in the blood, along with symptoms and findings on X-ray, are often used to indicate that a person has pancreatitis. A person with pancreatitis is also at risk of shock. Pancreatitis is often managed medically with analgesics, removal of gallstones or treatment of other causes, and monitoring to ensure a patient does not develop shock.
Cancer
Pancreatic cancer
Pancreatic cancers, particularly the most common type, pancreatic adenocarcinoma, remain very difficult to treat, and are mostly diagnosed only at a stage that is too late for surgery, which is the only curative treatment. Pancreatic cancer is rare in those younger than 40, and the median age of diagnosis is 71. Risk factors include smoking, obesity, diabetes, and certain rare genetic conditions including multiple endocrine neoplasia type 1 and herary nonpolyposis colon cancer among others. About 25% of cases are attributable to tobacco smoking, while 5-10% of cases are linked to inherited genes.
There are several types of pancreatic cancer, involving both the endocrine and exocrine tissue. Pancreatic adenocarcinoma, which affects the exocrine part of the pancreas, is by far the most common form. The many types of pancreatic endocrine tumors are all uncommon or rare, and have varied outlooks. However the incidence of these cancers has been rising sharply; it is not clear to what extent this reflects increased detection, especially through medical imaging, of tumors that would be very slow to develop. Insulinomas (largely benign) and gastrinomas are the most common types. In the United States pancreatic cancer is the fourth most common cause of deaths due to cancer. The disease occurs more often in the developed world, which had 68% of new cases in 2012. Pancreatic adenocarcinoma typically has poor outcomes with the average percentage alive for at least one and five years after diagnosis being 25% and 5% respectively. In localized disease where the cancer is small (< 2 cm) the number alive at five years is approximately 20%. For those with neuroendocrine cancers the number alive after five years is much better at 65%, varying considerably with type.
A solid pseudopapillary tumour is a low-grade malignant tumour of the pancreas of papillary architecture that typically afflicts young women.
Diabetes Mellitus
Type 1 diabetes
Diabetes mellitus type 1
Diabetes mellitus type 1 is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting cells of the pancreas. Insulin is needed to keep blood sugarlevels within optimal ranges, and its lack can lead to high blood sugar. As an untreated chronic condition, diabetic neuropathy can result. Type 1 diabetes can develop at any age but is most often diagnosed before adulthood. For people living with type 1 diabetes, insulin injections are critical for survival.
An experimental procedure to treat type 1 diabetes is the transplantation of pancreatic islet cells from a donor into the patient’s liver so that the cells can produce the deficient insulin.
Type 2 diabetes
Diabetes mellitus type 2
Diabetes mellitus type 2 is the most common form of diabetes. The causes for high blood sugar in this form of diabetes usually are a combination of insulin resistance and impaired insulin secretion, with both genetic and environmental factors playing an important role in the development of the disease. The management of type 2 diabetes relies on a series of changes in diet and physical activity with the purpose of reducing blood sugar levels to normal ranges and increasing insulin sensitivity. Biguanides such as metformin are also used as part of the treatment along with insulin therapy.
History
The pancreas was first identified by Herophilus (335–280 BC), a Greek anatomist and surgeon.[29] A few hundred years later, Rufus of Ephesus, another Greek anatomist, gave the pancreas its name. Etymologically, the term “pancreas”, a modern Latin adaptation of Greek πάγκρεας, [πᾶν (“all”, “whole”), and κρέας (“flesh”)], originally means sweetbread,[32] although literally meaning all-flesh, presumably because of its fleshy consistency. It was only in 1889 when Oskar Minkowski discovered that removing the pancreas from a dog caused it to become diabetic (insulin was later discovered by Frederick Banting and Charles Herbert Best in 1921).
The organ is mentioned prominently in the 1992 film Encino Man. Pauly Shore‘s character Stoney often refers to the organ in unrelated contexts, perhaps demonstrating a fundamental misunderstanding of what the pancreas does.
